Introduction
Sciatica is a term many have heard, yet few fully understand. Defined by the pain that radiates along the sciatic nerve, this condition affects countless individuals worldwide, impacting daily activities and overall quality of life. Delve with us into the journey of understanding sciatica, its causes, management strategies, and the path to recovery.
Understanding Sciatica: More Than Just Back Pain
Sciatica isn’t merely a backache; it’s a symptom indicating an underlying issue, most commonly a herniated disk, spinal stenosis, or a bone spur, compressing part of the nerve. This compression causes inflammation, pain, and often numbness in the affected leg, typically felt from the lower back to the buttock, then down the back of the leg.
Common Causes of Sciatica

1. Lumbar Herniated Disk: Also known as a slipped disk or ruptured disk. It’s the most common cause, where the soft inner material of the disk leaks out and irritates the adjacent nerve.
2. Degenerative Disk Disease: Aging can lead to wear and tear on the lumbar disks, causing inflammation and sciatica.
3. Bone Spurs and Spinal Stenosis: Overgrowth of bone or narrowing of the spinal canal can press on the nerve.
4. Spondylolisthesis: When one vertebra slips forward over another, it can compress the nerve.
5. Muscle Spasms: In the back or buttocks can compress the sciatic nerve.
Symptoms to Watch Out For
· Sharp pain that makes standing up challenging.
· Numbness, weakness, or difficulty moving the foot or leg.
· Constant pain in one side of the buttock.
· Pain worsened by sitting, but better when lying down or walking.
Sciatica Management and Treatment: A Holistic Approach
1. Physical Therapy: Tailored exercises can address underlying causes of sciatica. Strengthening the back muscles and improving posture can offer significant relief.
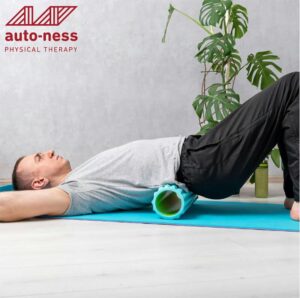
2. Foam rolling: This can provide relief and mobilize your lower back and paraspinal musculature.
3. Complementary Therapies: Acupuncture, chiropractic sessions, and massage therapy might provide relief for some.
4. Advanced Treatments: If conservative treatments don’t help, your doctor might suggest steroid injections, nerve root decompression surgery, or laminectomy depending on the cause.
Recovery and Prevention: Tips and Tricks
Regular Exercise: Focusing on the core muscles can help prevent sciatic pain by supporting the spine.
Proper Posture: When sitting, use a chair with good lumbar support. When lifting, use your legs, keeping the object close to your chest.
Stay Active: Prolonged inactivity can worsen your symptoms, so gentle movements and stretches are crucial.
Mind Your Sleep: Invest in a good mattress, and find a position that doesn’t put pressure on your lower back.
Lifestyle Adjustments for Long-Term Relief
1. Weight Management: Maintaining a healthy weight reduces the risk of sciatica.
2. Ergonomic Considerations: Ensure that your workspace, especially if you’re working from home, supports good posture.
3. Mind-body Techniques: Practices like yoga and meditation can help manage pain and are often recommended for sciatica patients.
Conclusion
Navigating the realm of sciatica requires patience, knowledge, and persistence. From understanding its root causes to implementing preventive strategies, the journey from diagnosis to recovery is paved with challenges but filled with hope. The road might be long, but with the right tools, guidance, and mindset, a pain-free future is within reach.
FAQs on Sciatica
1. What triggers sciatica?
Answer: Several factors can trigger sciatica, including lumbar herniated disc, degenerative disc disease, spondylolisthesis, spinal stenosis, muscle spasms in the back or buttocks, and even pregnancy. Activities such as heavy lifting or sudden movements can also lead to sciatica flare-ups.
2. How is sciatica diagnosed?
Answer: Sciatica is typically diagnosed through a combination of medical history review, physical examination, and if needed, imaging tests like MRI or CT scans.
3. Can sciatica go away on its own?
Answer: In many cases, sciatica can resolve itself within a few weeks. However, the underlying cause of the sciatica should be addressed to prevent future occurrences.
4. Are there exercises I can do to relieve sciatic pain?
Answer: Yes, exercises focused on strengthening and stretching the lower back, abdomen, and thighs can help alleviate sciatic pain. Physical therapists often recommend specific exercises tailored to individual needs.
5. How long does sciatic pain typically last?
Answer: Sciatica duration varies from person to person. For some, it can last a few days, while for others, it can persist for several weeks. Persistent or worsening pain should be discussed with a healthcare professional.
6. Is it okay to walk when suffering from sciatica?
Answer: Gentle walking can be beneficial for some people with sciatica. It can help improve flexibility and circulation. However, it’s essential to listen to your body and not push yourself too hard.
7. How do I differentiate between regular back pain and sciatica?
Answer: Sciatica is characterized by pain that radiates from the lower back down one or both legs, following the path of the sciatic nerve. It may also be accompanied by numbness, tingling, or weakness in the affected leg.
8. Is heat or cold better for sciatic pain?
Answer: Both can be beneficial. Cold packs can reduce inflammation when applied to the painful area, while heat packs can relax and soothe muscle tension.
9. Can sitting cause sciatica?
Answer: Extended periods of sitting, especially on a hard or uneven surface, can put pressure on the sciatic nerve and trigger symptoms.
10. Can stress or emotional factors affect sciatica?
Answer: Yes, chronic stress can lead to muscle tension and spasms, potentially triggering sciatic pain or exacerbating existing symptoms.


